January 16, 2023
SINGAPORE – A deadly form of brain cancer, glioblastoma, is nearly impossible to get rid of – even after patients undergo surgery to remove parts of the tumour, followed by chemotherapy, radiation therapy and other available treatments.
The average lifespan upon diagnosis is around two years. When the aggressive brain tumour returns after treatment, the cancer cells grow back with a vengeance, and the average lifespan is less than two years.
The recurrence rate for glioblastoma is close to 100 per cent, said Dr Yeo Tseng Tsai, head of the neurosurgery division at the National University Hospital (NUH).
But there is some hope as a research team from the National University of Singapore’s Yong Loo Lin School of Medicine (NUS Medicine) has developed a novel therapy targeted at aggressive tumours and cancer patients left with no options.
In a recent trial of the stem cell-based gene therapy in more than 60 cancer-stricken dogs and cats here, more than 80 per cent of them either lived past their original prognosis or had a better quality of life.
The researchers developed a technology to insert large amounts of therapeutic genes into stem cells that would react with antifungal drugs to target cancer cells.
Dr Yeo is looking to work with the NUS Medicine researchers to start clinical trials for recurrent glioblastoma patients in 2024.
Dr Sarah Ho, a senior research fellow at NUS Medicine’s biochemistry department who played a key role in developing the treatment, said her team can currently create enough modified stem cells for 18 human patients a week.
Dr Yeo, who is also a faculty member at NUS Medicine’s department of surgery, said: “There is a possibility that this novel and special form of therapy may help in prolonging the long-term survival of glioblastoma patients as its mechanism is different from existing therapies.
“It is also a form of precision cancer therapy as the suicide stem cells home in specifically on glioblastoma tumour cells, and not on normal brain cells.”
In Singapore, about 100 people are diagnosed with glioblastoma every year.
The treatment developed by Dr Ho and her team has also caught the attention of Dr Johnny Ong, a consultant at the National Cancer Centre Singapore (NCCS) who treats gastric, ovarian and colorectal cancers, among other illnesses.
In advanced stages, those cancers can spread to the peritoneum, the thin membrane surrounding organs in the abdomen. When multiple new tumours form on the membrane, patients will be afflicted with peritoneal carcinomatosis, a form of cancer with currently no effective treatments, said Dr Ong.
A key sign of this cancer is a swollen tummy, caused by fluids building up in the abdomen. Peritoneal carcinomatosis develops in 20 per cent of patients with gastric cancer, half of ovarian cancer patients and up to 10 per cent of colorectal cancer patients.
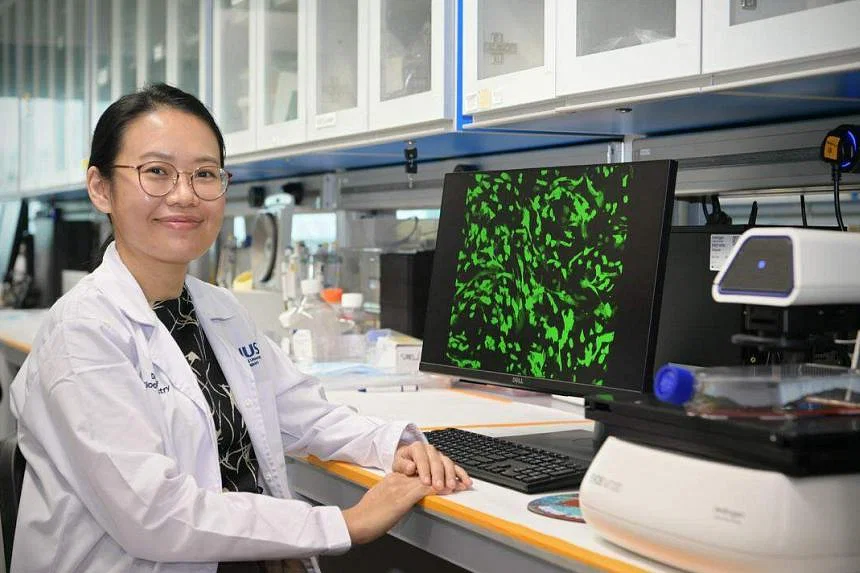
Dr Sarah Ho, a senior research fellow at NUS Medicine’s biochemistry department who played a key role in developing the treatment, said her team can currently create enough modified stem cells for 18 human patients a week. ST PHOTO: NG SOR LUAN
“The number of patients who can benefit from novel therapies targeting peritoneal carcinomatosis is huge,” said Dr Ong, who is from the department of sarcoma, peritoneal and rare tumours at NCCS.
Commenting on NUS Medicine’s therapy, Dr Ong said: “This form of targeted therapy is highly promising for peritoneal carcinomatosis. The direct delivery of the drug to the abdominal cavity reduces chances of the treatment leaking into other parts of the body, limiting potential side effects.” He envisions that the stem cell-based gene therapy can improve patients’ outcome, survival and quality of life.


