August 12, 2024
SINGAPORE – Bus driver Lee Chiow Jin left his hernia untreated for over two years, and it developed into a potentially life-threatening situation.
A hernia is a condition where part of an organ, such as the intestines, protrudes through a cavity wall. Causes include congenital defects, obesity and previous surgery.
The 48-year-old Singapore PR, who lives in Johor Bahru and travels daily to Singapore for work, had to rush to a hospital emergency room in February 2024 when the discomfort became too much to bear.
“There was a pulling sensation in my abdomen and I felt extremely bloated and uncomfortable. I had not been able to pass motion for two days,” said Mr Lee in an interview with The Straits Times in Mandarin.
It turned out that Mr Lee had an extremely rare case of not just one, but three hernias.
Two of them, known as inguinal hernias, had developed in the groin area, on both the left and right side.
The other was incisional hernia, where Mr Lee’s intestines got stuck along the weakened area of the scar from a prior colon surgery, causing pain and discomfort.
His intestines became blocked and inflamed, and would have burst, causing a serious infection.
In March, Mr Lee underwent an eight-hour surgery to repair all three hernias, in which Dr Marc Ong, consultant at Khoo Teck Puat Hospital’s (KTPH) general surgery department, employed a new surgical technique.
Called the enhanced-view totally extraperitoneal technique, or eTEP, the method involves closing the hernia defect and then inserting a mesh in the layers between the muscles to reinforce the repair.
“It was the most difficult operation that I’ve ever performed,” said Dr Ong, pointing to the number and position of the hernias.
KTPH is one of two public hospitals with a dedicated hernia surgery service, and Dr Ong has performed close to 20 operations in Singapore using the new eTEP technique since 2020.
National University Hospital is the other one with such a service.
“Mr Lee was lucky and did not have to go for an emergency operation, because somehow his intestines settled down after coming to the hospital,” Dr Ong said.
While Mr Lee’s previous colon surgery put him at risk of developing an incisional hernia, he was not obese and generally healthy.
Commenting on the rarity of the triple hernias, Dr Ong said: “He was just unfortunate to develop the three hernias simultaneously. This is a very rare occurrence which took place because he had a prior abdominal surgery which made him more susceptible to getting an incisional hernia.
“People who suspect they have hernia should seek clinical consultation earlier rather than wait till the hernia enlarges or becomes symptomatic.”
For two years, Mr Lee lived with hernia on the right side of his groin as it did not impact his daily life, and he wanted to avoid the pain of undergoing surgery. He was also unaware of the other two hernias.
“The hernia would only protrude out if I ran or coughed, and I would still be able to push the bulge back with my fingers,” said Mr Lee.
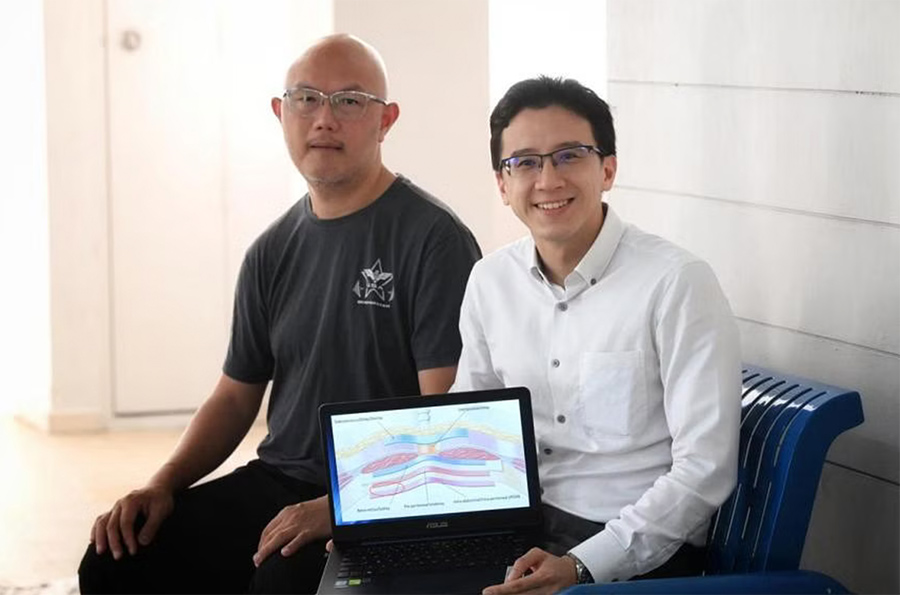
Dr Marc Ong (right) has performed close to 20 operations in Singapore using the new eTEP technique since 2020. PHOTO THE STRAITS TIMES
In traditional surgery, the mesh is put in the abdominal or peritoneal cavities – a space located within the abdomen and pelvis. This could lead to complications, such as formation of scar tissue, as the mesh comes into contact with organs like the intestines.
Traditional surgery is more costly as coated meshes, which are three times more expensive than uncoated meshes, have to be used to prevent the organs from sticking to the mesh.
In contrast, the surgical mesh can be held in place by the muscles with the eTEP technique.
Dr Ong, who went to Japan for a six-month training stint to learn the novel technique, said the most challenging part is to learn how to separate the muscle layers.
“It’s difficult because you must have a deep understanding of the anatomy to know where to create new spaces between the muscles. You also have to ensure you protect the muscle function too,” said Dr Ong, who is also the lead of hernia surgery at KTPH.
“Although the operation with the eTEP technique takes longer compared with the traditional method, post-operative pain is mild, and long-term mesh complications are said to be rare.”
To prepare for Mr Lee’s operation, Dr Ong planned the complex procedure with his Japanese mentor, Dr Kiyotaka Imamura.
It was meant to be done via keyhole surgery, where incisions were smaller, between 5mm and 1cm. If complications arise, there would be the option to do an open surgery, but that would mean a much bigger scar and longer downtime for the patient.
“During the operation, I found it difficult to split the muscles at one point. I did consider converting it to open surgery, but I decided to persist via keyhole approach as the operation was progressing safely,” said Dr Ong, who also credited the success of the surgery to the team he worked with.
Mr Lee was discharged four days after his operation and has made a full recovery since.
“After about a month, I was able to go back to my regular exercise routine like walking,” he added.